What is muscle tension dysphonia (MTD)?
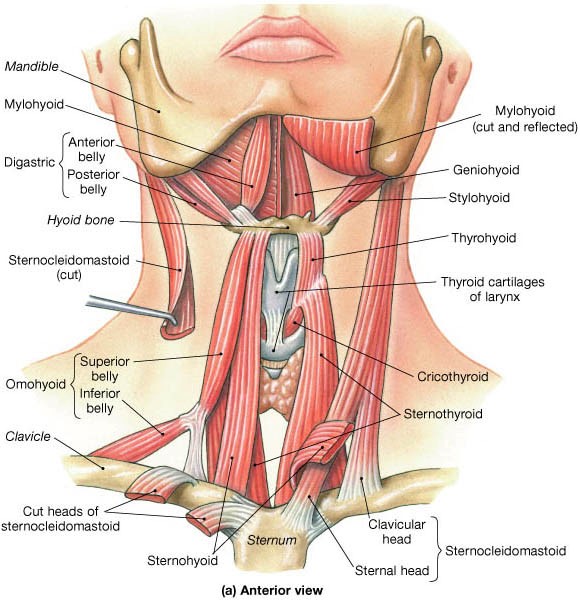
To understand MTD, it is probably best to begin thinking about how the voice works. There are muscles in the vocal cords (folds). In order for the voice to work, there should be some tension in these muscles. If they are too floppy, the voice can be weak. On the other side of spectrum, if the muscles are too tight, the voice will become strained and can even be painful. In addition to the muscles in the vocal cords (folds) there are muscles outside of the true voicebox (larynx) that are often involved in MTD. They are collectively called strap muscles and include the sternothyroid, sterhnohyoid, omohydoi, and even the sternocleidomastoid (see above). Patient’s often have soreness in the neck after speaking.
The actual word “dysphonia” comes from “dys—meaning wrong and “phonia” which comes from phonation—the process of making voice. So, if there is a problem with how the muscles and tissues function to make voice, we identify this as a dysphonia. In spasdmodic dysphonia, there are abrupt, unintentional movements (spasms) in the voice box that cause abnormal voice production (dysphonia).
Patients often describe their voices as “tight” or “strained” or sometimes even “choked.” This can sometimes be confused with spasmodic dysphonia. However, patients with MTD are less likely to have specific words that give them trouble and more often report that no matter what they say, it is tight.
Videostroboscopy, laryngeal EMG, and a complete voice evaluation can help make the diagnosis. Voice therapy to retrain the overused, tense muscles is by far the most effective way to treat MTD. Occasionally, patients have muscles that are so tight that muscle relaxants, sometimes even botox injections are helpful to get the muscle to relax enough to allow the patient to benefit from voice therapy.